Devices 101
The definitions and information you need to understand the complex device side of combination productsKnowledge, itself, is power, and understanding is the path to success.
In an effort to ensure the right questions are asked and the right information guides your progress, we have created a short-list of key topics that arise when pharmaceutical companies embark on new combination product ventures. The following are defined and explained below – feel free to click and jump or scroll through at your leisure.
Definition of Combination Products | Examples of Combination Product Devices | Device Requirements | Human Factors & Usability Engineering | Primary Mode of Action (PMOA) | Regulatory Submission Pathway | Device Platform | Governing Agencies | The European Commission’s MDR & IVDR | Commercial Teams | Glossary of Terms | Combination Product Case Studies
Combination Products can be cross-labeled (constituent parts sold separately), co-packaged (constituent parts packaged and sold together), or single-entry (chemically or physically combined constituent parts).
Examples of Combination Products with a Device Constituent Part
- Empty syringes packaged with a drug product
- Empty injection systems packaged with a drug product
- Transfer sets
- Lyophilized drug product vials packaged with reconstitution components.
- Surgical kits containing both a drug and a device to be used with it
- Prefilled syringes
- Prefilled auto-injectors
- Metered-dose inhalers
- Dry powder inhalers
- Nasal-spray
- Prefilled pumps
- Transdermal patch systems
- Prefilled iontophoresis system Microneedle “patch”
- Drug pills embedded with sensors
- Contact lens coated with a drug
- Drug-eluting stents
- Drug-eluting leads
- Condoms with spermicide
- Dental floss with fluoride
- Antimicrobial coated catheters/sutures
- Bone cements with antibiotics
- Live cells seeded on/in a device scaffold
- Extracorporeal column with column-bound protein
- Light-activated drugs/biological products labeled for use with a specific light source device
Device Requirements
Human Factors & Usability Engineering
Primary Mode of Action (PMOA)
The PMOA is the main therapeutic component that defines the combination product’s intended use. For drug delivery devices, that primary intended use will be attributed to either the drug part or the device constituent part of the combination product. For example, in a drug-eluting stent for opening diseased arteries, the PMOA is the device’s ability to open the artery. The drug provides a secondary PMOA as an “aid.” This designation as “primary” vs. “aid” helps determine through what regulatory body the combination product will be submitted. In the United States, a Combination Product with a PMOA related to the drug will be submitted to the Center for Drug Evaluation and Research (CDER); one related to the device will go to the Center for Devices and Radiological Health (CDRH).
Regulatory Submission Pathway
Consultants at Suttons Creek can guide you through both the development process and the submissions pathway. Governing bodies also supply guidance for your regulatory compliance.
Device Platform
Governing Agencies
Combination Products are regulated by various governing agencies, depending on where you plan to market them. Each will have its own set of complex rules and requirements. In this global marketplace, remaining compliant in an efficient and effective manner can be a very complicated puzzle to piece together.
For the United States of America, the US Food & Drug Administration (FDA) is the governing force. To serve as a focal point for all issues related to combination products, in 2002, the FDA created the Office of Combination Products (OCP). This office maintains compliance to all combination product related regulations and enforces the regulations outlined in the Current Good Manufacturing Practices (cGMP), which ensures that they are manufactured in a quality controlled environment.
For the European Union, the European Commission (EC) is the governing agency for combination products. Like the FDA’s OCP, the EC establishes and enforces combination product regulations for the safety of their constituents.
MDR and IVDR:
The European Parliament created and enforced the new Medical Device Regulation (MDR) and In Vitro Diagnostic Regulation (IVDR) in April 2017, replacing the Medical Device Directives (MDD) and the EU’s current Directive on in vitro diagnostic medical devices, in an effort to keep pace with the tremendous advancements and innovations in science and technology, to better protect patient safety, and to enhance transparency. It provides medical device manufacturers with a three-year window to implement compliance efforts before the May 2020 date of application (DOA) of the MDR and May 2022 DOA of the IVDR. Any medical device that is to be newly placed on the EU market after this date must comply with these new regulations.
- There is a broadening of the number and types of devices that are covered by the MDR. Cosmetic devices, as well as devices that have an ancillary use (e.g. devices that sterilize medical equipment), contact lenses and equipment for liposuction are now regulated under the MDR. Specifically, the MDR now officially defines a “medical device” as any “instrument, apparatus, appliance, software, implant, reagent, material, or other article intended by the manufacturer to be used, alone or in combination, for human being for one or more of the following specific medical purposes:
- Diagnosis, prevention, monitoring, predication, prognosis, treatment or alleviation of disease.
- Diagnosis, monitoring, treatment, alleviation of, or compensation for, and injury or disability.
- Investigation, replacement, or modification of an anatomical, physiological, or pathological process or state.
- Providing information by means of in-vitro examination of specimens derived from a human body, including organ, blood and tissue donations.
- With changes to the device classification rules, some devices are being reclassified to a higher risk class, such as surgical meshes and spinal implants, requiring more stringent and longer reviews as well as an increased need for clinical data. In fact, most software that was previously classified as a Class I medical device and self-certified will require Notified Body review under the MDR.
- The inclusion of a Unique Device Identification (UDI) mandate is another big change under the MDR. This will help make devices identifiable throughout the supply chain and sales region. Two identifiers are required, a device identifier that indicates the manufacturer and device, and a production identifier that indicates the production series/product batch.
- Notified Bodies must be assessed and designated to new higher standards under the Medical Device Regulation before they can conduct audits of manufacturers and reviews of medical devices. As a result, there will be fewer Notified Bodies available to review submissions and certify products, as well as more stringent oversight of their activities.
- Regulations concerning vigilance and post-market surveillance lead to the establishment of an EU database on Medical Devices, to correlate information from manufacturer, authorized representative, and importer. Information such as device registration, accredited Notified Bodies, Safety and Clinical Performance Reports, Serious Incidents, UDI, and Clinical Investigation Data will be captured.
- Stakeholders – suppliers, manufacturers, assemblers, subcontractors, distributors, importers, and EU Authorized Representatives – will assume larger, more defined responsibilities, as the new legislation Articles outline who is responsible for what obligations to conform to regulations. The Articles also newly require a qualified and experienced medical device expert available in the company and designated responsible for regulatory compliance.
Commerical Teams
The Commercial and marketing team is responsible for looking at how the final product (drug and device) will fit within the market. This includes availability of strategic alternatives, pricing requirements, patient population, willingness to use and pay for the product, patient capabilities, patient needs and wants, and competitive landscape. Commercial team inputs are critical to the success of a combination product and must start at initial strategy creation and work in alignment with the device development team through device selection, device design (including IFU and packaging), supply chain management, and launch and postmarket activites.
A short list of some key responsibilities that occur throughout the product development lifecycle are below:
Portfolio Management
- Market research – consumer and competitive landscape
- Market segmentation
- Building strategic case for having a particular drug delivery device
- Commercial viability of a device for the business
- Commercial goals – what does success look like in the market
- Provide feedback on customer needs
- Evaluate pricing plan with considerations for reimbursement and device costs/unit
Design + Development Planning
- Marketing plan
- Evaluation of device options
- Payor – rebates and discounts
- Demand planning
Device Design + Development
- Market research with current patients
- Market and brand-centric input into IFU
- Distribution strategy
Design Verification + Validation
- Launch strategy
- Set up patient resource hub (support hotline, website, training resources, FAQs, etc.)
Process Validation + Set Up
- Payor agreements
- Service level agreements
- Physician feedback / patient needs
- Ease of use of the product by the patient
- Pricing and contracting
- Patient support team / sales team trainings
Commercialization
- Patient training and support
- Patient adherence support
- Launch, postmarket, competitive monitoring
Glossary of Terms:
Applicable Standards List:
At the outset of Design and Development Planning including device selection for combination products, it is important to generate a comprehensive list of the standards applicable to the design of your combination product. This will act as one element of your Design Inputs along with other inputs such as User and Stakeholder Needs and Requirements, system-level requirements, commercial needs, and business needs.
Characterization Testing:
Initial testing of drug and device to derisk project and demonstrate working principles. May be used more specifically in a design of experiments if needed for determination of system parameters and test limits.
Complete Response Letter (CRL)
In United States pharmaceutical regulation, a complete response letter, per Code of Federal Regulations (CFR) 314.11, is a letter from the Food and Drug Administration (FDA), sent to an applicant indicating that their New Drug Application, Amended New Drug Application, or Biologics License Application is not approvable in its current state. The CRL will state the reason for the inability to approve, allowing the applicant to resubmit or withdraw the application or to request an opportunity for hearing.
Design and Development Plan:
“21 CFR 820.30(b) Design and development planning.
- Each manufacturer shall establish and maintain plans that describe or reference the design and development activities and define responsibility for implementation.
- The plans shall identify and describe the interfaces with different groups or activities that provide, or result in, input to the design and development process.
- The plans shall be reviewed, updated, and approved as design and development evolves.”
ISO 13485:2106 7.3.2:
“During design and development planning, the organization shall document:
- a) the design and development stages;
- b) the review(s) needed at each design and development stage;
- c) the verification, validation, and design transfer activities that are appropriate at each design and development stage;
- d) the responsibilities and authorities for design and development;
- e) the methods to ensure traceability of design and development outputs to design and development inputs;
- f) the resources needed, including necessary competence of personnel.”
Design History File (DHF):
A Design History File (DHF) is the collection of records (deliverables) that demonstrate that the product has been developed:
- In accordance with the DDP (if the DDP says something will happen, the DHF must provide evidence that it happened)
- In accordance with the Design Control Process (SOPs not just 820.30)
It can be electronic or paper based, a folder or an index of references and usually includes:
- Design and Development Plan
- Design Inputs/Outputs
- Design Verification Documentation
- Design Validation/Usability Engineering File
- Design Review Documentation
- Risk Management/Risk Management File
- Design Change Documentation
- Design Transfer Documentation
Design History File (DHF) Index:
This is an index of all materials to be created and planned for inclusion in the Design History File. It is optimally developed during planning/strategy stages at the outset of the project, not as a retroactive index of what came together at the end of development.
Design Review:
Design reviews, executed at various stages of combination product design and development, are required and documented per ISO 13485 (international) and 21 CFR 820.30 (US). It is important to document Minutes for each Design Review executed, to include in your Design History File.
21 CFR 820.30(e) Design review.
“· Each manufacturer shall establish and maintain procedures to ensure that formal documented reviews of the design results are planned and conducted at appropriate stages of the device’s design development.
- The procedures shall ensure that participants at each design review include representatives of all functions concerned with the design stage being reviewed and an individual(s) who does not have direct responsibility for the design stage being reviewed, as well as any specialists needed.
- The results of a design review, including identification of the design, the date, and the individual(s) performing the review, shall be documented in the design history file (the DHF).”
ISO 13485:2016
“At suitable stages, systematic reviews of design and development shall be performed in accordance with planned and documented arrangements to:
- a) evaluate the ability of the results of design and development to meet requirements;
- b) identify and propose necessary actions.
Participants in such reviews shall include representatives of functions concerned with the design and development stage being reviewed, as well as other specialist personnel.
Records of the results of the reviews and any necessary actions shall be maintained and include the identification of the design under review, the participants involved and the date of the review”
Design Trace Matrix:
A matrix designed to show the relationship between User Needs, Design Requirements, Design Specifications, Verification Evidence, and Validation Evidence. This is generated at the onset of Design and Development Planning and updated over course of the project.
Design Validation:
“21 CFR 820.3(z) Validation means confirmation by examination and provision of objective evidence that the particular requirements for a specific intended use can be consistently fulfilled.
(1) Process Validation means establishing by objective evidence that a process consistently produces a result or product meeting its predetermined specifications.
(2) Design Validation means establishing by objective evidence that device specifications conform with user needs and intended use(s).”
Design Validation Master Plan:
The overall plan for Design Validation defines how each design requirement is to be validated. This may include human factors data, clinical data, scientific literature, or other sources to validate the design.
“Design and development validation shall be performed in accordance with planned and documented arrangements to ensure that the resulting product is capable of meeting the requirements for the specified application or intended use.
The organization shall document validation plans that include methods, acceptance criteria and, as appropriate, statistical techniques with rationale for sample size.”
Design Validation Master Report:
This is a report of all validation activities. It is important additive information that supports the combination product’s regulatory filing.
Design Verification:
“21 CFR 820.3(aa) Verification means confirmation by examination and provision of objective evidence that specified requirements have been fulfilled.”
Design Verification Master Plan:
The overall plan for Design Verification defines how each design requirement is to be verified. This plan defines the available data that can be leveraged from the selected device manufacturer and provides any additional information (other than SOPs) necessary to develop Verification protocols.
ISO 13485:2016:
“The organization shall document verification plans that include methods, acceptance criteria, and, as appropriate, statistical techniques with rationale for sample size.”
Design Verification Master Report:
This is a report of all verification activities. It is important additive information that supports the combination product’s regulatory filing.
Device Master File:
Master Files, goverened by 21 CFR 814.20(c), is a comprehensive document that contains, or lists referenced available locations of, detailed information (including confidential information) pertaining to the manufacture, processing, packaging and storage of a drug delivery device system. Categorized as Type V for all device MFs by CBER, the DMF may be used to support the review of regulatory submissions and may include device specification, Quality assurance processses, production processes, manufacturing facilities, device components, materials, packaging/labeling, storage/maintenance details of the medical device.
Device Regulatory Plan / Strategy:
This document collects and defines the combination product strategy related to entering the combination product into a specific market that is regulated. This may include the required marketing submission for the jurisdiction, questions to address with regulators, meetings, the timing of regulatory interaction related to other engagement points, requirements specific to certain jurisdictions such as recognized standards or guidance, etc. This strategy is critical to program and submission success because it aligns the regulatory team on required combination product activities relative to regulatory interactions.
Drug Delivery System Specifications:
A System Specification, including drawings, bill of materials (BOM), and product specifications that, at a minimum defines the components. It is generated for the commercialization of the drug delivery device, informing purchase and production. While the Drug Delivery System Specifications are a Design Development Output, they may be updated during Design Transfer. Similarly, specifications designed to aid purchasing will be made for Labeling and for Packaging.
Failure Mode and Effects Analysis (FMEA):
This is a tool that can be used as part of the risk management process. An FMEA is a step-by-step approach for identifying all possible failures in a design (dFMEA), a manufacturing or assembly process (pFMEA), or use (uFMEA) of a combination product. Failures are prioritized according to severity, frequency, and/or detection. The outcome of the FMEA is to implement risk control measures to eliminate or reduce failures based on risk acceptance criteria.
Hazard Analysis (HA):
ISO14971:2022
“This document requires the manufacturer to compile a list of known and foreseeable hazards associated with the medical device in both normal and fault conditions and to consider the foreseeable sequences of events that can produce hazardous situations and harm.”
The Hazard Analysis consists of a list of all the hazards and hazardous situations associated with the medical device along with the sequence of events that can produce the hazardous situation. Often the Hazard Analysis will also include the severities assigned to particular harms. This analysis becomes part of the Risk Management File and feeds directly into the Risk Analysis.
Instructions For Use (IFU):
A form of labeling created by the market authorization holder for combination products that includes detailed user instructions. The IFU is reviewed and approved by regulatory bodies differently for a combination product than for a drug and has its own unique requirements. Complimentary written and visual instructions, formatted with the user population in mine, are suggested to cover everything between storage, preparation, administration, and disposal. For consideration tips on designing an effective IFU, click here. For content and format draft guidance from the FDA click here.
Quality Target Product Profile (TPP):
ICH Q8 Definition: “A prospective summary of the quality characteristics of a drug product that ideally will be achieved to ensure the desired quality, taking into account safety and efficacy of the drug product.”
A summary of the combination product’s characteristics that demonstrate and ensure desired quality, specifically related to the safety and efficacy of the drug or biologic behind delivered by the device. Device considerations should be included. Industry evidence indicates that programs with a QTPP have higher approval rates.
Risk Management Plan (RMP):
The creation and oversight of the RMP lies with the Market Authorization Holder and cannot be delegated. It is officially defined as:
ISO 14971:2022 4.4:
“Risk management activities shall be planned. For the particular medical device being considered, the manufacturer shall establish and document a risk management plan in accordance with the risk management process. The risk management plan shall be part of the risk management file.
This plan shall include at least the following:
- a) the scope of the planned risk management activities, identifying and describing the medical device and the life cycle phases for which each element of the plan is applicable;
- b) assignment of responsibilities and authorities;
- c) requirements for review of risk management activities;
- d) criteria for risk acceptability, based on the manufacturer’s policy for determining acceptable risk, including criteria for accepting risks when the probability of occurrence of harm cannot be estimated;
NOTE 1 The criteria for risk acceptability are essential for the ultimate effectiveness of the risk management process. For each risk management plan the manufacturer needs to establish risk acceptability criteria that are appropriate for the particular medical device.
- e) a method to evaluate the overall residual risk, and criteria for acceptability of the overall residual risk based on the manufacturer’s policy for determining acceptable risk;
NOTE 2 The method to evaluate the overall residual risk can include gathering and reviewing data and literature for the medical device being considered and similar medical devices on the market and can involve judgment by a cross-functional team of experts with application knowledge and clinical expertise.
- f) activities for verification of the implementation and effectiveness of risk control measures; and
- g) activities related to collection and review of relevant production and post-production
NOTE 3 See ISO/TR 24971[9] for guidance on developing a risk management plan and on establishing criteria for risk acceptability.
NOTE 4 Not all parts of the plan need to be created at the same time. The plan or parts of it can be developed over time.
If the plan changes during the life cycle of the medical device, a record of the changes shall be maintained in the risk management file.”
Usability Engineering (Human Factors) Integration Plan:
Defines all Human Factors activities ahead of the project, proactively identified for the fulfillment of IEC 62366. Having this plan tends to be an important review factor with regulators.
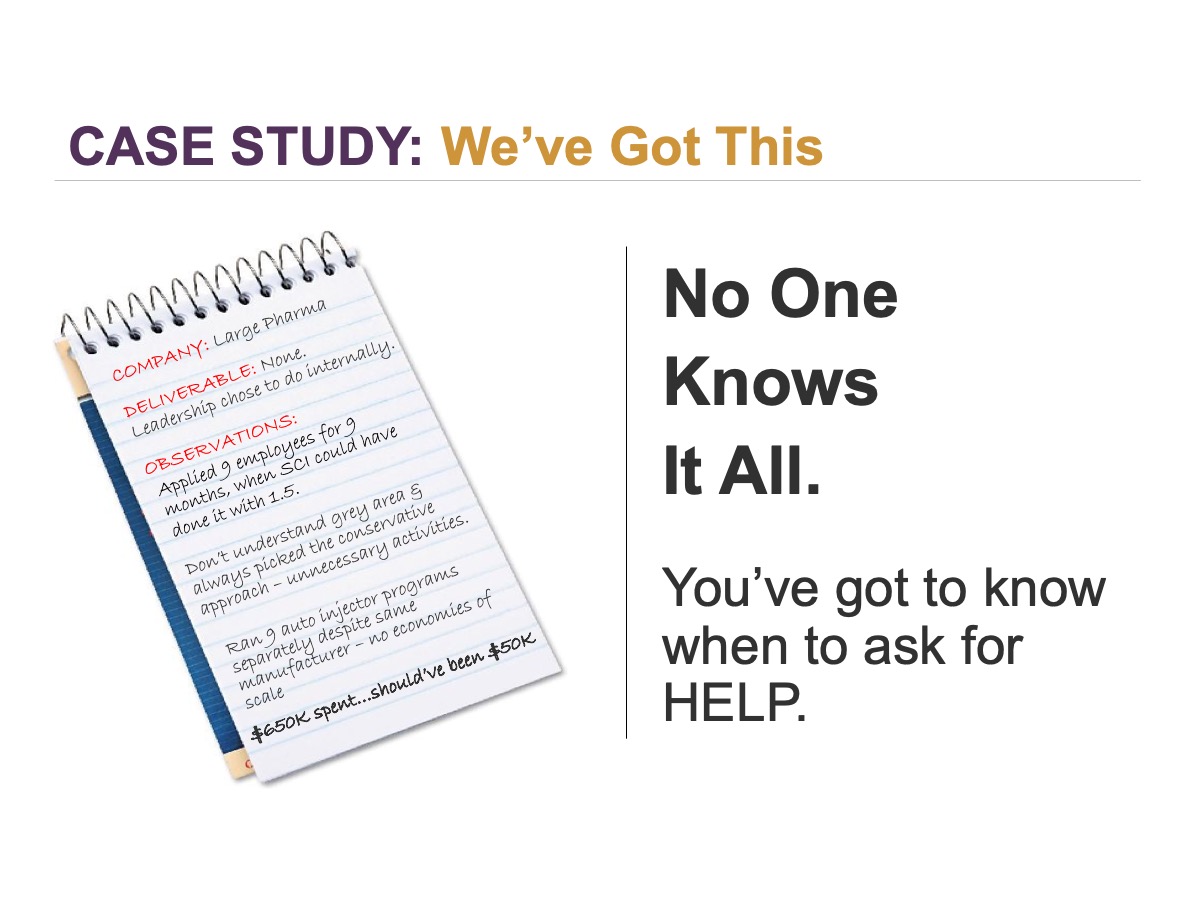
Combination Product Case Studies
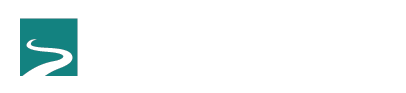
Device Platforms & Small Pharma:
“The Knowledge Gap”
In this case study, we observe a small pharma company that needed to execute a combination product development program. Upper management was in full support of providing resources to get the job done right, but they didn’t have the experience and knowledge to give effective direction to their teams. The first step toward success is knowing what you don’t know and seeking out those answers, so this small pharma was on the right track.
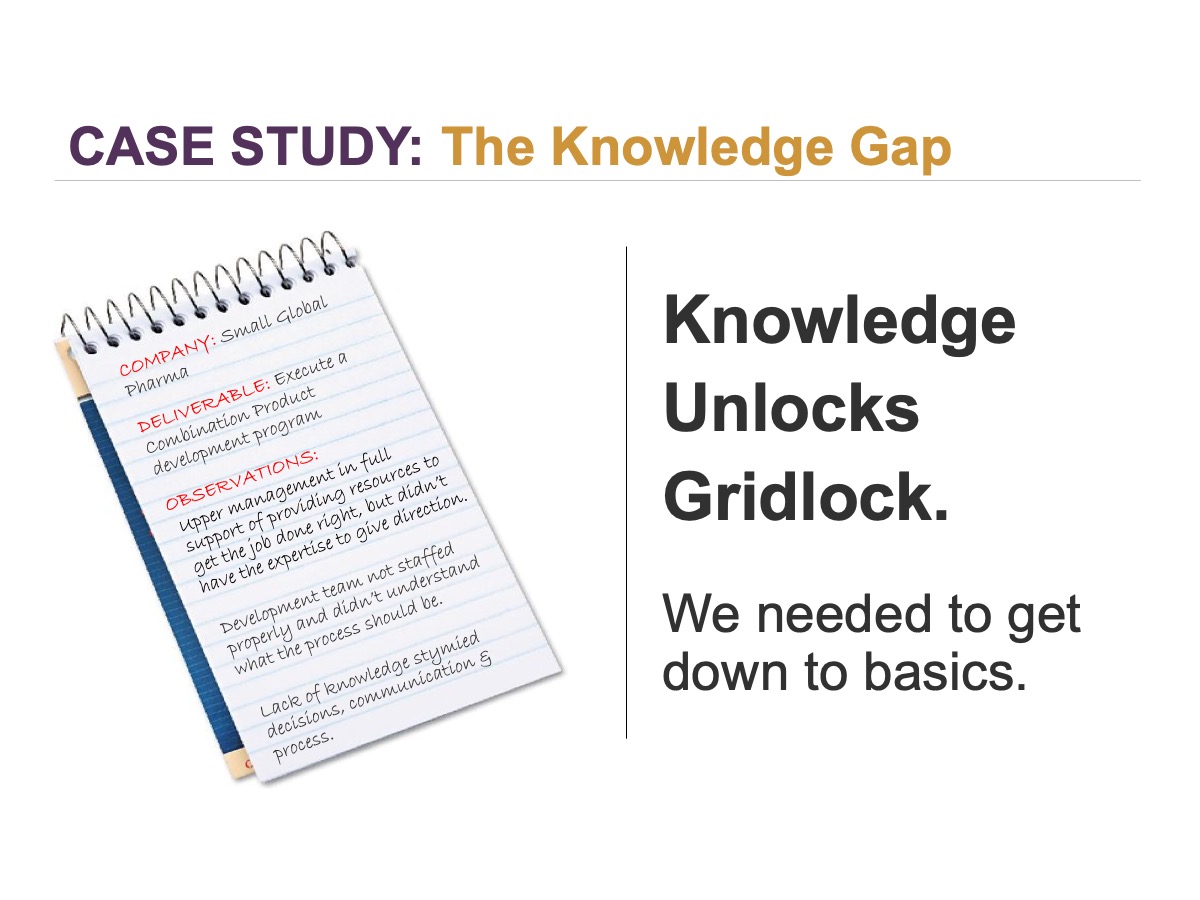
Device Platforms & Big Pharma:
“United We Stand”